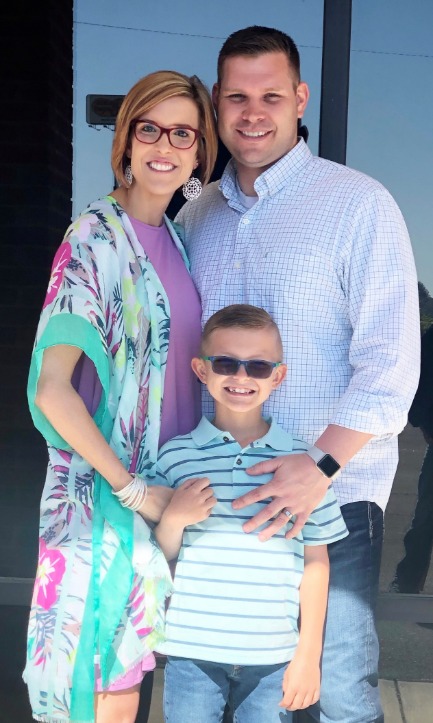
At just 32 years old, Ashley Rochester is in the prime of her life. She and her husband, Nathan, who she started dating in high school, have been married for 10 years. Together they have an 8-year-old son, Easton. As a busy mom who also works full-time as a Certified Medical Dosimetrist at Erlanger’s Cancer Center, Ashley stays on the move while keeping up with her son’s activities. In 20 15, Ashley started to experience pelvic pain and other issues that started with a 9 cm ovarian cyst.
“When my doctor surgically removed the cyst, she commented that I had some large varicosities in my pelvis, but it never registered in my mind that those enlarged veins might be contributing to the terrible pelvic pain I was experiencing,” remembers Ashley. “After the cyst was removed, my pain continued, and I had so much pressure and swelling, especially the week before and during my menstrual cycle. So I felt like I only had two weeks out of the month that I felt somewhat okay, the other two were miserable.”
For several years, Ashley did her best to ignore the dull pain, pressure, and occasional constipation as well as the intense pain she felt after having any type of intimate moments with her husband.
“I felt too young to be going through this, but I didn’t know what to do,” says Ashley. In January 2019 Ashley ended up in the emergency room, where a pelvic ultrasound picked up the presence of these enlarged veins. A CT scan was quickly ordered to provide more information and ultimately confirmed that she in fact had extremely large pelvic varicosities.
Ashley met with Dr. Michael Greer, vascular surgeon with University Surgical Associates.


He diagnosed her with pelvic vein congestion, a condition that occurs when pelvic veins become swollen and painful due to low blood flow – like the varicose veins that can develop in your legs. Pelvic vein congestion is often the result of pregnancy and the pressure put on the pelvis from carrying a baby.
Women with multiple pregnancies are at even higher risk. Dr. Greer recommended a procedure called pelvic vein embolization, a non-surgical, minimally invasive approach that relieves the heaviness, pressure and chronic pelvic pain.
A NON-SURGICAL PROCEDURE
During pelvic vein embolization, a venogram is performed where a small catheter is inserted to inject a dye into the dilated vein, providing a road map of what’s happening inside. A synthetic material or medication called an embolic agent is used to seal off the abnormal blood vessels. Sometimes coils are used to block larger vessels, causing blood to be rerouted to other smaller veins and relieve pressure caused by stagnant blood flow. Pelvic vein embolization is a highly effective way of blocking the blood vessel, without the need for open surgery – resulting in less pain and a quicker recovery than an open procedure.
“During the procedure, I discovered that in addition to a problem with her left ovarian vein, Ashely’s left iliac vein was almost completely compressed, which required a stent to be placed to restore proper blood flow,” says Dr. Greer. “When a stent is needed during this procedure, it takes a little longer to recover from any cramping and discomfort, usually lasting less than a week.”
“Because of the stent, I stayed in the hospital overnight so that they could appropriately observe and monitor the post-operative pain and discomfort. Otherwise I would have more than likely gone home the same day,” says Ashley. “I was uncomfortable due to some muscle spasms, probably from the stent, and had little twinges of pain in my back and pelvis for three or four days. After a week, I was feeling pretty good and already noticing a drastic improvement in my pre-operative symptoms. After three or four months, all of these symptoms were completely gone and I felt 110% better!
COMFORTING AND COMPASSIONATE CARE
While under the care of Dr. Greer and his team, Ashley felt comforted, accommodated and cared for completely. From the front desk all the way to the surgical team, the experience was top-notch. “Dr. Greer and his nurse practitioner Mary Ann took so much time talking with me, explaining the procedure, answering my questions and helping me feel comfortable throughout the entire process,” says Ashley. “If you are experiencing these symptoms of pelvic pain, bloating and discomfort and you can’t find a cause, you definitely need to see a vascular surgeon like Dr. Greer. I wouldn’t hesitate to have this surgery again.”
Since her surgery and recovery, Ashley notes that several aspects of her life have dramatically improved. In addition to the restored intimate relationship she has with her husband, Ashley most enjoys the fact that she can live an active life without reservation.
“I wouldn’t feel good day to day and it really interfered with our lives. Our family enjoys being outdoors and we would be at the lake, spending time on the water, and I would have to stay back at the camper while Nathan and Easton went out on the Jet Ski because I did not feel well. That’s not true anymore,” says Ashley. “Instead of always having to sit down and rest, I’m activity participating in my life. Now I can do what I want to do.”
Don’t let pelvic pain interfere with living your life! If you think you may have pelvic vein issues, click here to take our free online vein assessment or call (423) 267-0466 to schedule a consultation today.



Leave A Comment