Pancreatic cancer is an elusive type of cancer that affects 60,000 Americans each year. It can be scary and confusing if you or a loved one is diagnosed with this largely silent disease process.
Alan Koffron, MD, fellowship-trained hepatobiliary surgeon with University Surgical Associates, explains what pancreatic cancer is, pancreatic cancer risks, warning signs you shouldn’t ignore, and available pancreatic cancer screening and advanced treatment options.
What Is Pancreatic Cancer?
Pancreatic cancer is a very aggressive form of digestive cancer. Adult men and women of all ages, races, and demographics can develop this deadly disease. However, it is more widespread in men and African Americans. While cancer tends to be more prevalent as we age, people in their 40s, 50s and 60s are more commonly diagnosed with pancreatic cancer.
Pancreatic cancer develops when an abnormal growth of cells grows in the pancreas, a hormone-producing gland located between the stomach and the spine near the small intestine.
There are two types of pancreatic cancer:
Exocrine (Pancreatic Adenocarcinoma): This is the most common type of pancreas cancer. It develops in the cells that line the ducts of the pancreas that produce digestive enzymes.
Endocrine (Islet Cell Tumors): This type of pancreas cancer begins in the hormone-producing cells of the pancreas and occurs less frequently.
Pancreatic cancer is the third most common cause of cancer-related death in the US. This high ranking is partially because pancreas cancer seldom has symptoms in stage 1 or stage 2.
If symptoms do appear, it is usually when cancer has already progressed to stage 3 or stage 4. For many people diagnosed (approximately 30 percent), the cancer cells have already spread before symptoms become noticeable.
What Causes Pancreatic Cancer?
Like most cancers, it’s unknown what causes pancreatic cancer. But we do know there are risk factors that can cause cells to become cancerous.
Some people inherit gene changes that raise their risk of pancreatic cancer. These are called inherited gene mutations. However, most people aren’t born with these gene mutations; they are acquired after birth due to environmental factors and poor lifestyle choices.
Sadly, many gene mutations are random and occur without any external cause.
A family history of both pancreas cancer and pancreatitis increases your chances of developing pancreatic cancer.
Other non-biological risk factors that have been scientifically proven to increase your chances of acquiring the gene mutations that cause pancreatic cancer include:
- Tobacco Use
- Obesity
- Diabetes
- Chronic Pancreatitis
- Chronic Inflammation of the Pancreas
Of all of these risk factors, smoking is the most dangerous. Roughly 25% of pancreatic cancers are believed to be caused by cigarette smoking.

What Are The Symptoms of Pancreatic Cancer?
The pancreas is deep inside the body, so even if you have regular check-ups at your doctor, early tumors can’t be seen or felt during routine physical exams.
Many people have pancreatic cancer for years before developing any symptoms. Once symptoms develop, in most cases, the tumor has become very large, or the cancer cells have already spread to other organs.
When pancreatic cancer symptoms do appear, they are often vague or similar to most other pancreatic diseases.
“The first signs of pancreatic cancer are typically abdominal or back pain that doesn’t go away, or the skin becomes jaundiced or yellow. Other symptoms include nausea, diarrhea, bloating and stool changes, along with loss of appetite, elevated blood sugar, weight loss and general fatigue,” Dr. Koffron says.
These symptoms, especially aches and pains, can come and go. And because most could occur due to a variety of minor conditions or other diseases, you can see why people go years before diagnosis.
“Because pancreatic cancer is much easier to treat when it’s found early, it’s important to pay attention to your body’s signals and talk to your doctor if something’s not right,” says Dr. Koffron.
How Is Pancreatic Cancer Diagnosed?
Pancreatic cancer can’t be diagnosed in an exam, even in its latest stages and if the tumor is large, because the pancreas is very deep in the abdomen.
Typically, a patient is already experiencing symptoms that flag a doctor to perform pancreatic cancer screening tests, scans, and imaging to diagnose or rule out pancreatic cancer.
Many of these tests can also be used as pancreatic cancer screening tools for those without symptoms but who are at high risk for developing pancreatic cancer. If someone has a strong family history of pancreatic cancer, doctors can use these tests to potentially find cancer early and when it is more treatable.
The most common way pancreatic cancer is discovered is with imaging tests. There are numerous ways a doctor might want to create these pictures of the inside of your body. The three most common are:
- Computed Tomography (CT) Scans
- Endoscopic Ultrasound (EUS)
- Magnetic Resonance imaging (MRI)
Unfortunately, these screening modalities are not 100 percent effective in finding small lesions, pre-cancer or early-stage cancers.
There are also blood tests some doctors order to help diagnose pancreatic cancer. Labs your doctor might request include:
- Liver Function Tests
- Tumor Markers (CA 19-9 or CEA levels)
- CBC Chemistry Panel
Pancreatic Cancer Treatment Options
Pancreatic cancer is a complicated condition to treat, specifically because it’s usually advanced by the time it is diagnosed.
Another challenge in treating pancreatic cancer is the pancreas’ location. Although it’s not a large organ, it’s deep in the abdomen and nestled right next to the blood vessels that feed other major organs and lymph nodes that make insulin and digestive enzymes. Its location alone makes it a technically demanding surgery to perform.
“The hope for any cancer – including pancreatic – is to surgically remove it using safe but aggressive techniques. When the cancer is contained within the pancreas and hasn’t spread to surrounding tissue, surgery is the mainstay of treatment,” Dr. Koffron says. “For tumors that are larger and beginning to grow but haven’t spread to other organs, we often use neoadjuvant chemotherapy, which means chemo that’s administered before surgery. It’s used to shrink or slow the tumor’s growth so it becomes possible to remove. For individuals whose disease has spread outside of the pancreas, chemotherapy and radiation are used to prolong survival.”
How To Prevent Pancreatic Cancer?
A person’s average lifetime risk of developing pancreatic cancer is about 1 in 65.
Unfortunately, there is no sure way to prevent pancreatic cancer. There are risk factors such as age, gender, race, and family history that you can’t control. But you can drastically reduce your risk and help prevent pancreatic cancer by eliminating scientifically proven risk factors in your control.
Don’t Smoke or Use Tobacco: The risk of getting pancreatic cancer is about twice as high among people who smoke than those who have never smoked. If you smoke or use tobacco products, it is crucial that you quit immediately.
Maintain a Healthy Weight: If you are overweight, weight loss should be a top priority. Carrying excess body fat increases your chances of cancer. Aim to stay at a healthy weight through regular exercise and a healthy diet free of processed foods and too much sugar. Follow a diet with plenty of fresh fruit, vegetables, whole grains, and lean meat.
Avoid or Limit Alcohol: Clinical trials have linked heavy alcohol use to pancreatic cancer. Drinking alcohol in excess can also lead to chronic pancreatitis, which is known to increase pancreatic cancer risk.
Limit Exposure to Chemicals: Some research indicates that heavy metals and compounds found in pesticides, industrial products such as CHC solvents, and even some beauty products and foods may be linked to a gene mutation in some patients with pancreatic cancer. More research needs to be done, but to be safe, you should limit your exposure to these chemicals when possible.
What You Can Do to Support Yourself or a Loved One with Pancreas Cancer
When diagnosed with cancer, it can not only take a toll on you physically; it can be emotionally draining and affect your mental health. This can be true for the person with cancer and their caregivers, family and close friends.
If you have been diagnosed with pancreas cancer, joining a support group is one of the best ways to help process and manage the wide range of emotions that come with a cancer diagnosis.
If you are the loved one of a person with pancreas cancer, there are many ways you can offer care and support.

Going through cancer can be an emotional roller coaster with many ups and downs. Be sensitive to your loved one’s feelings.
If you are the primary caregiver of someone with pancreatic cancer, you are a very important part of the cancer patient’s care team. This can take a toll both emotionally and physically. You must care for yourself too.
Why Choose A Pancreatic Cancer Specialist?
Although we know pancreatic cancer treatment is complex, the diagnosis isn’t an automatic death sentence – particularly when you choose a surgeon with the experience and education needed to offer the very latest and most effective treatment options.
“It’s important for people to know that we have the most advanced cancer-fighting surgeries and treatments right here in Chattanooga. In the last 15 years or so, surgical fellowships that focus on the techniques and procedures of the liver and pancreas allow us to do very technically difficult operations on a routine basis,” Dr. Koffron says. “The outcomes are better when you seek care from a pancreatic cancer specialist at a high-volume center – meaning one that does more than 20 operations a year, which is what we do here at Erlanger. But more than that, you have access to a dedicated surgical and recovery care team and other cancer specialists who are all working together to fight your cancer and help you live a longer and healthier life.”
If you or a loved one has been diagnosed with pancreatic cancer, you have choices when it comes to your surgeon and your treatment options. For more information or to schedule an appointment, call 423-267-0466.
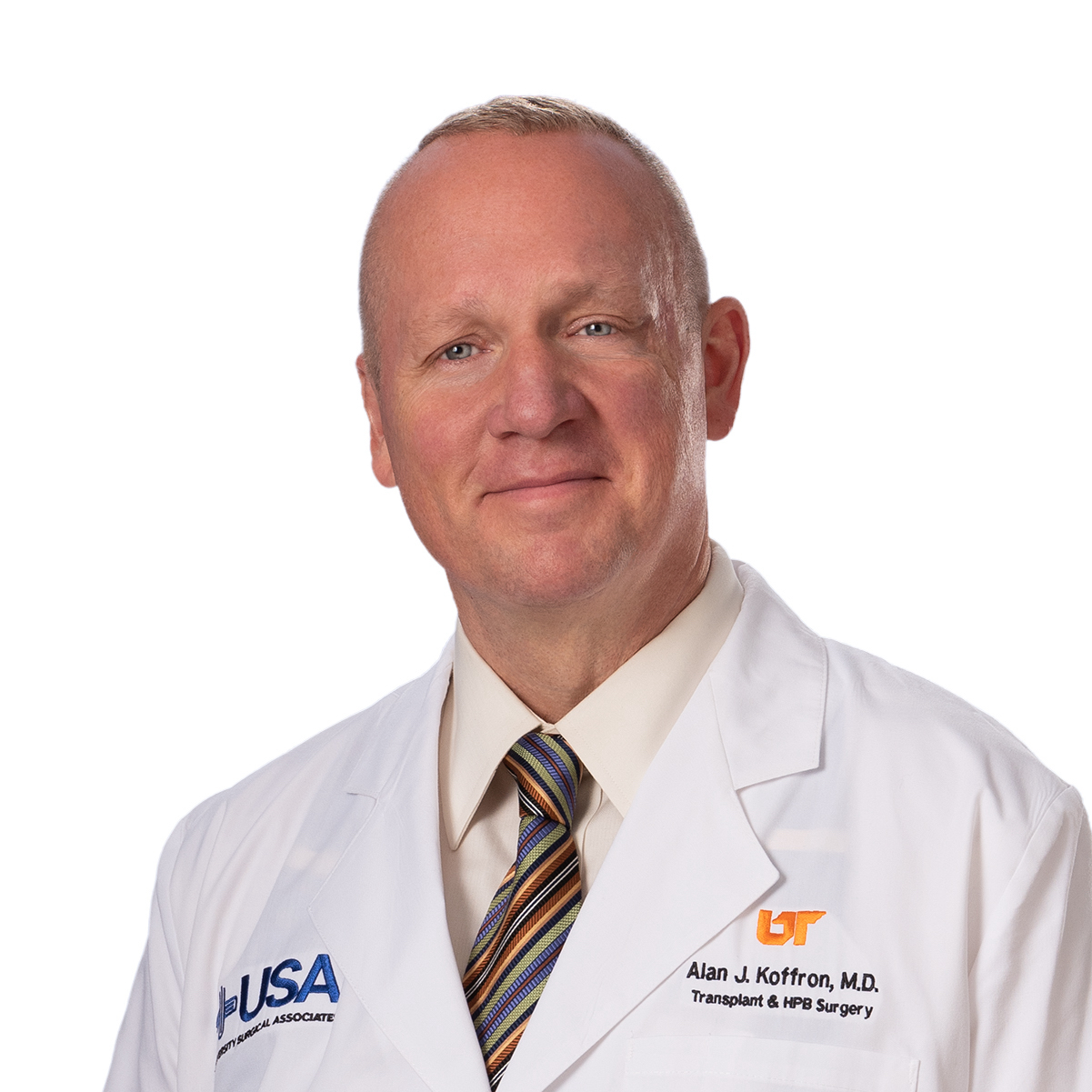
Dr. Koffron is a fellowship trained multiple-organ transplant and hepatobiliary surgeon who specializes in liver and kidney transplant and advanced surgical treatment of conditions of the liver, pancreas and biliary system. He serves as Surgical Director, Erlanger Kidney Transplant Center.
Dr. Koffron is certified by the American Board of Surgery and fellow of the American College of Surgeons. He sees patients at the USA Surgical Specialties Building. Click here to learn more about Dr. Koffron’s education and experience.



Insightful article! Pancreatic cancer surgery plays a crucial role in the treatment and care of individuals diagnosed with this challenging disease. Understanding the intricacies and advancements in surgical techniques is essential for patients and their families. It’s encouraging to see comprehensive information provided, which promotes better understanding and empowers individuals to make informed decisions. By increasing awareness and knowledge about pancreatic cancer surgery, we can contribute to improved patient outcomes and support those affected by this condition.